Interleukin-10 Polymorphisms in Association with Prognosis in Patients with B-Cell Lymphoma Treated by R-CHOP
Article information
Abstract
Interleukin-10 (IL10) plays an important role in initiating and maintaining an appropriate immune response to non-Hodgkin lymphoma (NHL). Previous studies have revealed that the transcription of IL10 mRNA and its protein expression may be infl uenced by several single-nucleotide polymorphisms in the promoter and intron regions, including rs1800896, rs1800871, and rs1800872. However, the impact of polymorphisms of the IL10 gene on NHL prognosis has not been fully elucidated. Here, we investigated the association between IL10 polymorphisms and NHL prognosis. This study involved 112 NHL patients treated at the National Cancer Center, Korea. The median age was 57 years, and 70 patients (62.5%) were men. Clinical characteristics, including age, performance status, stage, and extra-nodal involvement, as well as cell lineage and International Prognostic Index (IPI), were evaluated. A total of four polymorphisms in IL10 with heterozygous alleles were analyzed for hazard ratios of overall survival (OS) and progression-free survival (PFS) using Cox proportional hazards regression analysis. Diffuse large B-cell lymphoma was the most common histologic type (n = 83), followed by T-cell lymphoma (n = 18), mantle cell lymphoma (n = 6), and others (n = 5). Cell lineage, IPI, and extra-nodal involvement were predictors of prognosis. In the additive genetic model results for each IL10 polymorphism, the rs1800871 and rs1800872 polymorphisms represented a marginal association with OS (p = 0.09 and p = 0.06) and PFS (p = 0.05 and p = 0.08) in B-cell lymphoma patients treated with rituximab plus cyclophosphamide, doxorubicin, vincristine, and prednisone (R-CHOP). These findings suggest that IL10 polymorphisms might be prognostic indicators for patients with B-cell NHL treated with R-CHOP.
Introduction
The incidence rate of hematologic malignancies has steadily increased during recent decades in many regions. Non-Hodgkin lymphoma (NHL) is the most frequent hematologic cancer type, accounting for 43% of all hematologic malignancies and 90% of lymphomas [1]. In Korea, the incidence of NHL is approximately 10.8 per 100,000 persons per year [2]. The risk of NHL is increased by age, chronic infection, and genetic and environmental factors [3].
The frequency of B-cell lymphoma is higher than that of T-cell lymphoma in NHL, and the survival rate of B-cell lymphoma has continuously improved. The prognosis varies, depending on patient age, clinicopathological features, and genetic factors. The International Prognostic Index (IPI) is the most commonly used tool to predict the prognosis of NHL [45]. However, its efficiency could be enhanced by the inclusion of additional prognostic markers.
Interleukin-10 (IL-10), one of the Th2 anti-inflammatory cytokines, is mainly secreted by type 2 helper T-cells (Th2) and activates T-cells and monocytes, as well as B lymphocytes. IL-10 can promote cancer by immunosuppression or stimulation of cell proliferation (B-cells and Th2-cells) and plays an important role in the regulation of inflammation by suppressing the release and function of Th1 pro-inflammatory cytokines [6]. Recent evidence suggests that the imbalance of the Th1/Th2 response induced by genetic variants affects the pathogenesis of NHL [7]. These findings indicate that IL10 polymorphism may be a principal mediator cytokine in the pathogenesis of NHL.
The IL10 gene is positioned on chromosome 1 (1q31–1q32). Previous studies have revealed that the transcription of IL10 mRNA and its protein expression may be influenced by some single-nucleotide polymorphisms (SNPs) in the promoter region, including rs1800896, rs1800871, and rs1800872 [78].
However, the impact of polymorphisms of the IL10 gene on NHL prognosis has not been fully elucidated. Here, we investigated the association between IL10 polymorphisms and NHL prognosis.
Methods
Patients and collection of clinical data
This study recruited 112 patients diagnosed with NHL at the National Cancer Center in Korea from 2005 to 2012. Patients gave informed consent, which was approved by the institutional review board. Inclusion criteria were as follows: (1) ethnically Korean; (2) available samples at diagnosis; and (3) diagnosed with non-Hodgkin lymphoma on the basis of World Health Organization (WHO) guidelines [9], with or without treatment with an rituximab plus cyclophosphamide, doxorubicin, vincristine, and prednisolone (R-CHOP) regimen. There were no recruitment restrictions with regard to gender or cancer stage. The mean age of patients was 56 years, and 62.5% of cases were male.
Chemotherapy was repeated every 3 weeks for a total of six to eight cycles, as decided by the clinician. After every three cycles, the therapeutic response was evaluated. Follow-up was performed every 3 months for the first 2 years; thereafter, the interval was extended to every 6 months. Information on demographic characteristics, including age, IPI, performance status by WHO, cancer stage, and extra-nodal involvement, were evaluated and analyzed.
Candidate polymorphisms and genotyping
Five polymorphism sites were selected, based on a review of the literature and a genetic database. We searched the literature using the keywords ‘IL-10, polymorphism, and cancer’ in 3 years and decided to include five SNPs (rs1800896, rs1800871, rs1800872, rs3021094, and rs1554286), which are located in the promotor and intron regions of the IL-10 gene. These SNPs have been reported as having a significant association with cancer more than once out of 45 publications. Among them, rs1800896 was excluded from the analysis, because its minor allele frequency (MAF) was 0.027. Genomic DNA was extracted from patients' peripheral blood using a QIAamp DNA Blood Mini Kit (Qiagen, Valencia, CA, USA), and SNPs were genotyped using a Taqman 5' nuclease assay for allelic discrimination with commercially available Taqman probes (Applied Biosystems, Foster City, CA, USA), according to the manufacturer's instructions. Briefly, genotyping reactions were carried out in a volume of 5 µL, containing 10 ng of genomic DNA, 2.5 µL of TaqMan Genotyping Master Mix (Applied Biosystems), and genotyping probe, in a 384-well plate. Genotyping results were analyzed with an ABI 7900HT Sequence Detection System (Applied Biosystems) by applying allelic discrimination plots using SDS 2.1 software (version 5.0; Applied Biosystems). Genotyping results were confirmed by independently replicating genotyping reactions for 10% of the samples, and all genotypes were the same.
Statistical analyses
Associations between clinicopathological factors, including age, IPI, performance status by WHO, cancer stage, and extra-nodal involvement, and patients' survival were analyzed using univariable or multivariable Cox proportional hazards regression models.
All polymorphisms were in Hardy-Weinberg equilibrium, with p-values greater than 0.05 using HWE.test in R package {genetics} [10].
Three different genetic models—additive, dominant, and recessive—were used to assess each SNP's effect on the hazard ratios (HRs) for survival. Overall survival (OS) was calculated from the day of diagnosis to the day of last follow-up or death. Progression-free survival (PFS) was measured from the day of diagnosis to the day of progression or death. Patients who were alive at the time of follow-up were censored. The effects of SNPs on OS or PFS were presented as HRs and 95% confidence intervals (CIs). The total patient dataset was used for the analysis. The same analysis was repeated using the diffuse large B-cell lymphoma (DLBCL) patients treated by R-CHOP. All reported p-values are two-sided, and statistical analyses were performed using SAS version 9.3 (SAS Institute Inc., Cary, NC, USA).
Results
Clinical characteristics of NHL patients and treatment outcomes
The associations between clinical characteristics and OS or PFS are summarized in Tables 1 and 2. The most common histologic type was DLBCL (n = 83); others included T-cell lymphoma (n = 18), mantle cell lymphoma (n = 6), and others (n = 5). Univariable results showed age, gender, performance status, extra-nodal involvement, and IPI as being significantly associated with OS and PFS in the total patient dataset, with p-values less than 0.05. Variables that were significant in the univariable results were used in the multivariable analysis. Using the backward variable selection method in the multivariable model, male, performance status 2, and extra-nodal involvement were highly associated with a poor prognosis for OS and PFS equally. In addition, age was also significantly associated with PFS. A subgroup analysis using DLBCL patients treated by R-CHOP showed a similar trend, except for age and performance status, as the multivariable result for PFS.
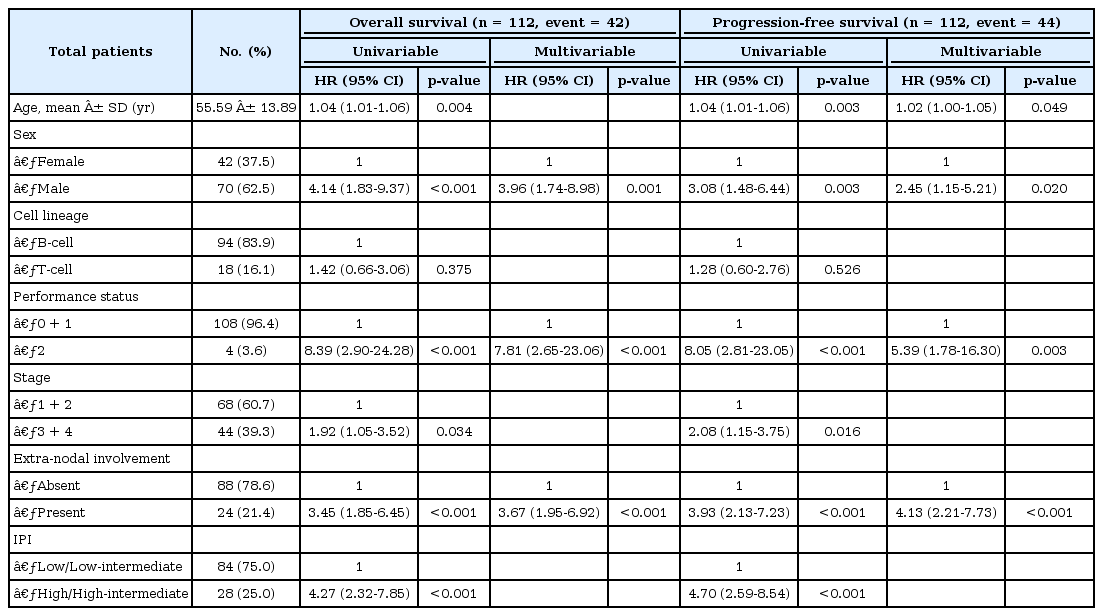
HRs of clinical characteristics of patients with non-Hodgkin lymphoma for overall survival and progression-free survival (n = 112)
IL10 polymorphisms and survival
Genotype frequencies of four SNPs in the IL10 gene are listed in Tables 3 and 4. The MAF of rs1800872 was the highest among the four SNPs.
Of the four polymorphisms, rs1800871 and rs1800872 of the IL10 gene represented a marginal association with both OS (p = 0.094 and p = 0.058) and PFS (p = 0.051 and p = 0.077) (Tables 3 and 4) in B-cell lymphoma patients treated by R-CHOP, based on additive models. Using an additive model for the reference allele, the HR for rs1800871 was 0.64 times for OS (95% CI, 0.38 to 1.08) and 0.60 times for PFS (95% CI, 0.36 to 1.00) as one minor allele increases in B-cell lymphoma patients treated with an R-CHOP regimen (Tables 3 and 4).
Discussion
This study showed that rs1800871 and rs1800872 of IL10 were marginally associated with the prognosis in NHL. Especially among the subtypes of NHL, these two polymorphisms had a decreased risk with the minor allele for DLBCL. It suggests that IL10 polymorphisms might be prognostic indicators for such patients.
There have been many reports on the relationship between IL10 gene polymorphisms and the risk of lymphoma, including meta-analyses. These studies reported that IL10 (rs1800890, rs1800896, rs1800871, and rs1800872) polymorphisms are associated with the risk of NHL.
These polymorphisms had a significantly increased risk for DLBCL and follicular lymphoma [1112]. These results showed the opposite effects compared with our study. However, all of the polymorphisms were not associated with the risk of NHL. In another study, the rs1800896 reference allele was associated with an increased risk of NHL. On the other hand, rs1800871 and rs1800872 had no association with the risk of NHL [13].
For an association with clinical outcomes, a previous study reported that IL10 gene polymorphisms influenced OS in T-cell lymphoma NHL [14]. In another study, IL10 genotypes were associated with a lower production of anti-inflammatory Th2 cytokines as a factor influencing an unfavorable course of NHL [15]. However, the other study showed no difference of allele frequencies between lymphoma patients and healthy controls, and moreover, they did not show any association of OS or event-free survival with IL10 genotypes [16].
Our study has several limitations. Our study has a limited number of patients. Furthermore, these subtypes, such as mantle cell lymphoma and T-cell lymphoma, were not common, and fewer studies reported an association between IL10 gene polymorphisms and these subtypes. Therefore, the sample size was limited, and the statistical power may be insufficient.
Although our study has a limited number of patients, it gave us implications for the association of IL10 genotypes and the prognosis of B-cell lymphoma treated by R-CHOP, which is a standard therapy. Thus, we need to further study this on a large scale to confirm these results.
Acknowledgments
This work was supported by grants from the National Cancer Center of Korea (NCC-0510410) and the National Research Foundation of Korea (NRF), funded by the Korean government (MSIP) (2014R1A2A2A01002553).


