3. Sulkava S, Muggalla P, Sulkava R, Ollila HM, Peuralinna T, Myllykangas L,
et al. Melatonin receptor type 1A gene linked to Alzheimer's disease in old age. Sleep 2018;41:zsy103.



4. Huang HC, Jiang ZF. Accumulated amyloid-β peptide and hyperphosphorylated tau protein: relationship and links in Alzheimer’s disease. J Alzheimers Dis 2009;16:15–27.


5. LaFerla FM, Oddo S. Alzheimer’s disease: Aβ, tau, and synaptic dysfunction. Trends Mol Med 2005;11:170–176.


6. Litvinchuk A, Wan YW, Swartzlander DB, Chen F, Cole A, Propson NE,
et al. Complement C3aR inactivation attenuates tau pathology and reverses an immune network deregulated in tauopathy models and Alzheimer's disease. Neuron 2018;100:1337–1353.



8. Zhang B, Gaiteri C, Bodea LG, Wang Z, McElwee J, Podtelezhnikov AA,
et al. Integrated systems approach identifies genetic nodes and networks in late-onset Alzheimer's disease. Cell 2013;153:707–720.



9. Jiang W, Zhang Y, Meng F, Lian B, Chen X, Yu X,
et al. Identification of active transcription factor and miRNA regulatory pathways in Alzheimer's disease. Bioinformatics 2013;29:2596–2602.



10. Pinero J, Ramirez-Anguita JM, Sauch-Pitarch J, Ronzano F, Centeno E, Sanz F,
et al. The DisGeNET knowledge platform for disease genomics: 2019 update. Nucleic Acids Res 2020;48:D845–D855.

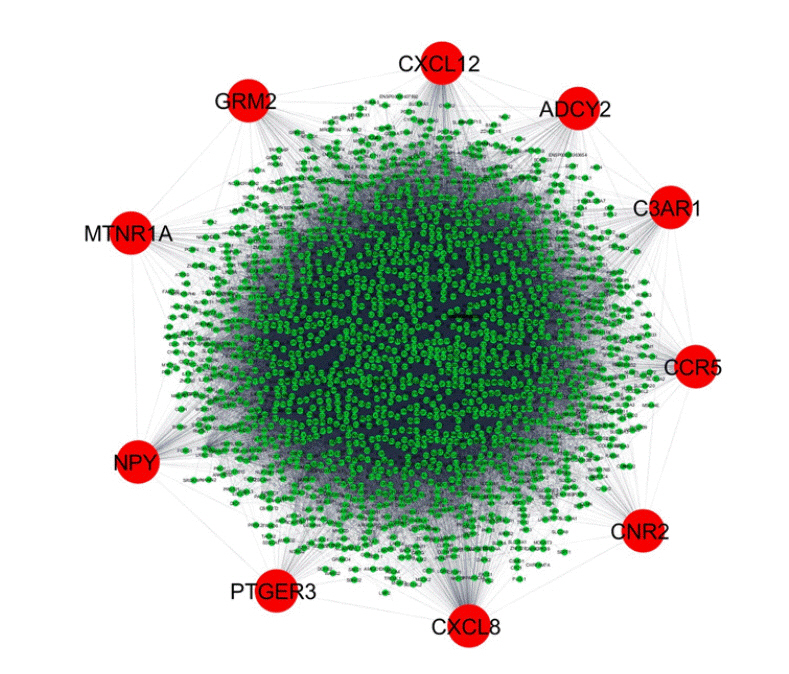
11. Shannon P, Markiel A, Ozier O, Baliga NS, Wang JT, Ramage D,
et al. Cytoscape: a software environment for integrated models of biomolecular interaction networks. Genome Res 2003;13:2498–2504.



12. The UniProt Consortium. UniProt: a hub for protein information. Nucleic Acids Res 2015;43:204–212.

13. Szklarczyk D, Gable AL, Lyon D, Junge A, Wyder S, Huerta-Cepas J,
et al. STRING v11: protein-protein association networks with increased coverage, supporting functional discovery in genome-wide experimental datasets. Nucleic Acids Res 2019;47:D607–D613.



14. Chin CH, Chen SH, Wu HH, Ho CW, Ko MT, Lin CY. cytoHubba: identifying hub objects and sub-networks from complex interactome. BMC Syst Biol 2014;8 Suppl 4:S11.


15. Pathan M, Keerthikumar S, Ang CS, Gangoda L, Quek CY, Williamson NA,
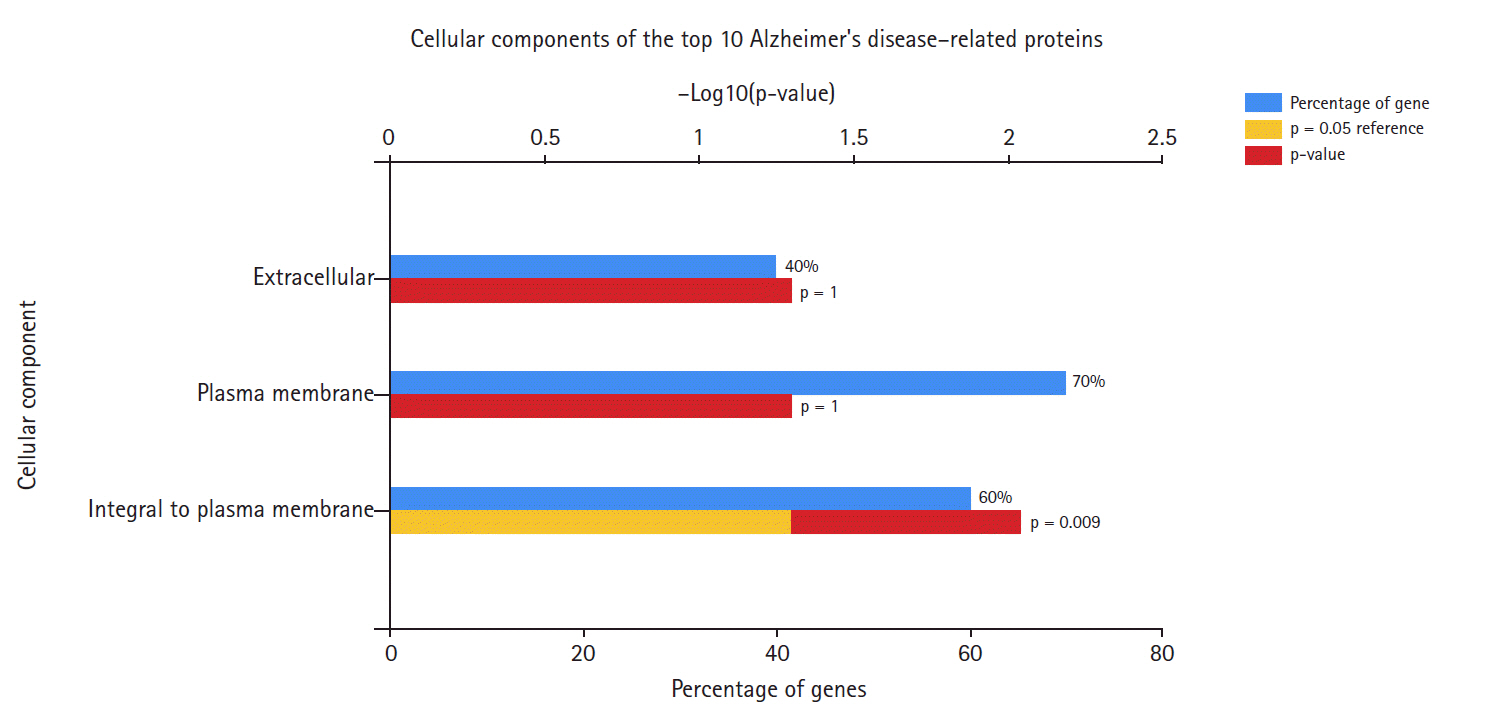
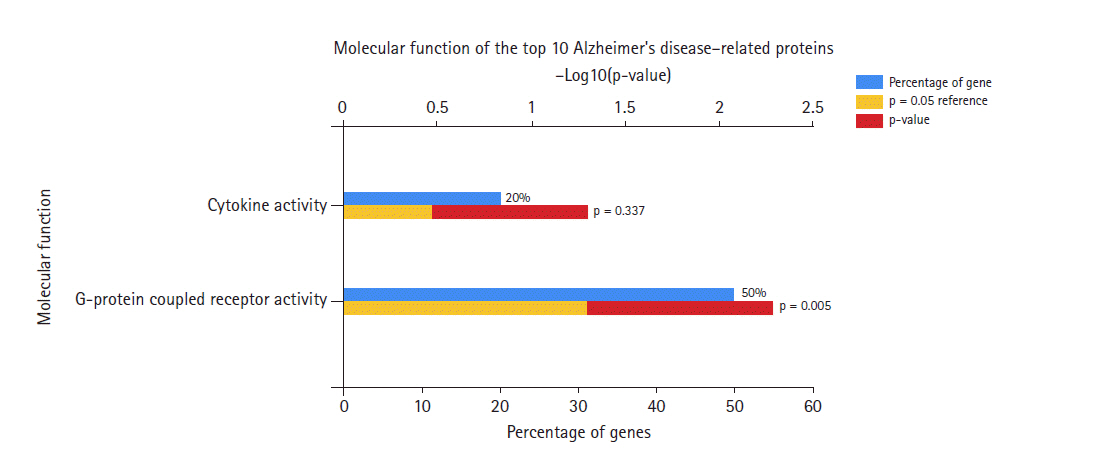
et al. FunRich: an open access standalone functional enrichment and interaction network analysis tool. Proteomics 2015;15:2597–2601.


16. Maingret V, Barthet G, Deforges S, Jiang N, Mulle C, Amedee T. PGE2-EP3 signaling pathway impairs hippocampal presynaptic long-term plasticity in a mouse model of Alzheimer's disease. Neurobiol Aging 2017;50:13–24.


17. Slawik H, Volk B, Fiebich B, Hull M. Microglial expression of prostaglandin EP3 receptor in excitotoxic lesions in the rat striatum. Neurochem Int 2004;45:653–660.


18. Koide S, Onishi H, Hashimoto H, Kai T, Yamagami S. Plasma neuropeptide Y is reduced in patients with Alzheimer's disease. Neurosci Lett 1995;198:149–151.


19. Grammas P, Roher AE, Ball MJ. Increased accumulation of cAMP in cerebral microvessels in Alzheimer's disease. Neurobiol Aging 1994;15:113–116.


20. Bezzi P, Domercq M, Brambilla L, Galli R, Schols D, De Clercq E,
et al. CXCR4-activated astrocyte glutamate release via TNFalpha: amplification by microglia triggers neurotoxicity. Nat Neurosci 2001;4:702–710.



23. Combarros O, Infante J, Llorca J, Pena N, Fernandez-Viadero C, Berciano J. The chemokine receptor CCR5-Delta32 gene mutation is not protective against Alzheimer's disease. Neurosci Lett 2004;366:312–314.


24. Micale V, Mazzola C, Drago F. Endocannabinoids and neurodegenerative diseases. Pharmacol Res 2007;56:382–392.


25. Richards G, Messer J, Faull RL, Stadler H, Wichmann J, Huguenin P,
et al. Altered distribution of mGlu2 receptors in beta-amyloid-affected brain regions of Alzheimer cases and aged PS2APP mice. Brain Res 2010;1363:180–190.


33. Xiang S, Huang Z, Wang T, Han Z, Yu CY, Ni D,
et al. Condition-specific gene co-expression network mining identifies key pathways and regulators in the brain tissue of Alzheimer's disease patients. BMC Med Genomics 2018;11:115.



35. Wu M, Fang K, Wang W, Lin W, Guo L, Wang J. Identification of key genes and pathways for Alzheimer’s disease via combined analysis of genome-wide expression profiling in the hippocampus. Biophys Rep 2019;5:98–109.